Lupus affects around half a million people in Europe. This chronic auto-immune disease affects multiple organs throughout the body, and patients with lupus undergo periods where the disease is active – so-called ‘flare phases’ – and where they have barely any symptoms – remission. Lupus is a lifelong condition, and although there is no cure for lupus, there are existing treatments that alleviate symptoms and prevent flares. However, despite an improvement in treatments available today, there is only a 40-45% chance that patients will respond well to those treatments. For all of these reasons, new and better therapies are needed for lupus patients.
The 3TR project is using molecular techniques (like transcriptomics) to examine gene expression pathways in patients as they transition from remission to flare and vice-versa. By comparing the patterns that they find to similar patterns seen in other auto-immune diseases, it’s hoped that the project can unearth new insights into the molecular basis of auto-immune diseases which could lead to better treatments for patients.
“What we want in the 3TR project is to be able to follow these patients and then verify, validate or find new insights into how patients behave from the transcriptomic point of view when it comes to their flares or their remission,” says Marta Alarcón Riquelme, the project coordinator for 3TR, who is Scientific Director and researcher in Functional Genomics at GENYO centre for Genomics and Oncological Research from the Fundación Pública Andaluza Progreso y Salud (FPS).
Using data from a 2000-person strong molecular dataset on patients with lupus from a previous IMI project, PRECISESADS, the 3TR project looked at data from 321 patients in various stages of flare-up and remission and successfully identified molecular signalling pathways that could distinguish people who were having active flare-ups from those who were experiencing low disease activity or complete remission from the disease. This was the first time that these molecular signalling pathways have been shown to distinguish disease activity levels in lupus patients.
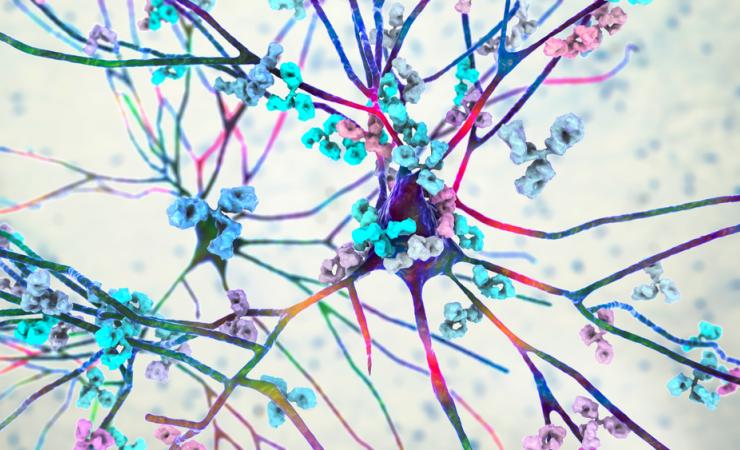
A recently published peer-reviewed paper demonstrated that people who are in an active disease state showed increased activity along inflammatory and interferon (proteins that help the body to fight infection) pathways. This meant that people who were having flare-ups were experiencing constant active immune responses. When you’re sick, having an active immune system is a good thing, but in lupus patients the immune system is overactive and can cause damage in the body’s own tissues and organs.
For patients that were in remission or a low disease activity state, the inflammatory pathways were not active – instead, inhibitory pathways were shown to be activated, protecting the body against malfunctioning immune system responses.
Molecular biosignatures informing treatment selection
The results of this study show that examining the molecular characteristics of lupus patients could be a better way to identify treatments than the current methods, which are largely trial-and-error based and are focused on reacting to the different organs that present symptoms.
“Looking at the previous studies done under the frame of 3TR using the data from PRECISEADS, we could see that molecular patterns did not align with the disease manifestations in lupus patients, meaning that different pathways can be activated even when clinical symptoms are similar,” says Ioannis Parodis of the Karolinska Institutet in Sweden, who led the study.
“You could see a variety of molecular aberrances irrespective of which organ was involved. This told us that we needed to start thinking in molecular terms when we do therapeutic decision-making.”
Validation, verification and unpacking the data
The next step for the 3TR project is to carry out a longitudinal study which will verify the work done in this paper. The study will also verify a computer model which has been devised to predict the immune response of a person with lupus based on their molecular signature.
It’s a challenge – “there are very few datasets, if any, of longitudinal lupus patients that have transcriptome data available,” says Alarcón Riquelme.
One problem is that it is difficult to find patients that are only taking one drug to combat lupus – many patients are taking a variety of medications to combat the various symptoms that they are experiencing across several organs.
“Treatments interfere with the patient’s biology and gene expression,” says Parodis. “It is really difficult to get clean data.”
Cleaner data might be easier to obtain if we knew more about hydroxychloroquine, a drug taken by the majority of lupus patients.
“With the knowledge we have today, all patients with lupus should be on hydroxychloroquine,” says Parodis. “It has multiple benefits for the patients in the long run. It protects against cardiovascular complications, it prevents flares, it’s associated with less progression to organ damage.”
The 3TR project is embarking on a separate study that will examine a subset of patients that are only taking this drug and nothing else. The results of this study will help to demystify the transcriptome patterns and molecular signatures of patients who are taking a combination of medications – because the effects caused by hydroxychloroquine will be known, and can be removed from the analysis.
Applying the results: to clinical practice and other diseases
Central to 3TR’s work is the applicability of these results to real-world hospital settings. Since testing for elevated protein levels is easier for clinicians to conduct compared to gene expression, another study on the cards for the 3TR lupus team is one where the results from the gene expression analysis can be paired to protein levels.
“We want to make this amenable for use in routine clinical practice,” says Parodis. “Treatment recommendations are to date based on clinical endpoints, not molecular endpoints.”
Shared similarities at the molecular level between patients with lupus and other immune-mediated diseases like rheumatoid arthritis and asthma might mean that grouping these diseases together makes sense for future clinical trials where a drug candidate targets one specific molecular pathway that they have in common.
“There are inflammatory pathways that are very similar between some of these diseases,” says Alarcón Riquelme. “If you have patients with different diseases that share a similar pathway, then you might be able to do basket clinical trials.”
These findings may provoke a breakthrough not only for lupus, but for these other diseases too.
3TR is supported by the Innovative Medicines Initiative, a partnership between the European Union and the European pharmaceutical industry.