Lung cancer is the most common cause of cancer-related death worldwide – 1.8 million people died from lung cancer in 2020.
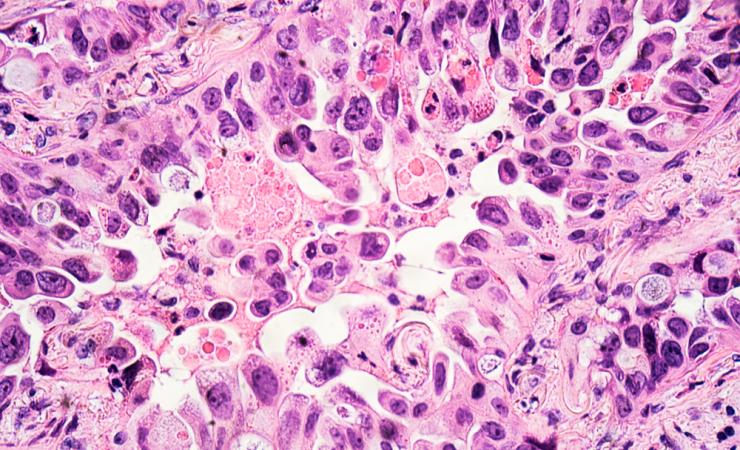
The most common kind of lung cancer is non-small-cell lung cancer (NSCLC), which is sometimes caused by a BRAF gene that is functioning incorrectly. Mutations in the BRAF gene typically switch a protein on but never switch it off, so that cells keep dividing unchecked, leading to a tumour.
Recent developments in cancer therapies have highlighted that BRAF mutations can be targets for therapies. This seems to work for BRAF mutant lung cancer, where a combination of dabrafenib-trametinib for the treatment of BRAF-mutant NSCLC has been approved by the European Medicines Agency and the US Food and Drug Administration.
However, some patients seem to develop resistance to this combination of drugs, so the CANCER-ID project set out to understand why. One hypothesis that they tested was whether the resistance to dabrafenib-trametinib was associated with BRAF mutation.
The project carried out a smattering of molecular analyses on patients with advanced lung cancer. In particular, they used a technique called single circulating tumour cell (CTC) sequencing. Ninety circulating tumour cells were sequenced and this was the first time that CTCs had been molecularly profiled for their resistance to BRAF-targeted therapies. However, only one of those cells contained a BRAF mutation which suggests that resistance to BRAF inhibitors treatments may not be driven by BRAF-mutation.
The researchers also carried out whole genome analysis and investigated several cancer-related pathways. They selected 141 genes that were determined to be of greatest relevance and observed a wide range of diversity involving different mechanisms.
CANCER-ID was supported by the Innovative Medicines Initiative, a partnership between the European Union and the European pharmaceutical industry.